The side effects of cancer-related treatments and surgeries can be rough, whether it’s chemo-induced nausea, constipation caused by painkillers, or insomnia brought about by general anxiety.
Enter cannabis. Both controversial and widely praised, it can be challenging to figure out if, how, and when to incorporate cannabis into your treatment plan, especially with legal limitations or a lack of support from medical professionals. Nearly two-thirds of more than 50 Breasties who used cannabis during treatment said they did not work with their medical team to do so.
The Breasties Guide to Cannabis is here to help inform and navigate, as you explore the potential benefits and drawbacks of using cannabis during cancer-related treatments and surgeries.
Disclaimer: Recommendations shared on The Peak are not replacements for medical advice. Everyone is different and what works for one Breastie may not work for another. We always recommend checking with your medical team before using any new products, supplements, or medications in conjunction with or instead of prescribed treatments.
What is Cannabis, THC, and CBD?
The basics: cannabis is a psychoactive substance, commonly referred to as marijuana, that comes from the cannabis plant.
Tetrahydrocannabinol, or THC, is the main psychoactive ingredient in the plant, though it is not the only chemical, or cannabinoid, found in cannabis that can have an impact on our central nervous system and be used for medicinal purposes. For example, Cannabidiol, or CBD, is equally reported to have therapeutic effects without impacting consciousness. Synthetic cannabinoids are also available.
Using cannabis medicinally is far from new, with the first reported use dating back to China around 2700 BC. Other historical evidence includes a European “ninth-century medical text, the Old English Herbarium, [which] advised pounded hemp for dressing wounds and a liquid concoction ‘for pain of the innards.’”
Medicinal cannabis is legal in nationwide Canada and in 37 of the 50 United States, while cannabis is also legal recreationally for adults in Canada and in 19 states.
However, there is little consensus on the use of cannabis in medical settings.
“There are a lot of gaps in the evidence and further studies are needed to understand the short- and long-term benefits of cannabis and its cannabinoids,” explains Simran Malhotra M.D., a triple board-certified physician specializing in palliative care and lifestyle medicine and a BRCA1 previvor.
Additionally, the lack of standardization and oversight of cannabis products adds another layer of complexity for both patients and healthcare providers, according to Cannabis and Cannabinoid-Based Medicines in Cancer Care, a guide developed with the objective of “addressing the use of cannabinoids in advanced cancer and palliative care patients and provide the necessary guidance to clinicians.”
Dr. Malhotra explains that there are some FDA-approved medications that contain cannabinoids and that “most states only allow medical cannabis for patients who have specific chronic, debilitating, or terminal illness diagnoses.”
Why Use Cannabis for Cancer-Related Treatments?
Through Dr. Malhotra’s palliative care practice, she sees patients who “have debilitating symptoms that may not respond to first-or second-line conventional treatments,” and then ask about cannabis use in hopes of improving their quality of life.
While cannabis cannot be recommended for curing cancer or as a substitute for primary treatment regimens, it has been found to be “highly efficient in managing cancer-related symptoms in patients,” such as nausea, vomiting, loss of appetite, anxiety, and cancer-related pain.
However, Dr. Malhotra points out, “it comes with an array of potential side effects.”
She explains that these side effects can range from physiologic, like low blood pressure, drowsiness, and dry mouth, to psychologic, such as euphoria, confusion, poor concentration, and anxiety.
These symptoms, she continues, “are typically dose-related and worse in the elderly.”
Long-term complications can include lung problems, such as bronchitis, lung cancer, cannabinoid hyperemesis syndrome, and neuropsychiatric symptoms, Dr. Malhotra explains. Smoking cannabis is not recommended due to adverse pulmonary effects.
“It is important to weigh the potential risks and benefits before making a decision about using cannabis or cannabinoids,” Dr. Malhotra says, stressing the importance of patients both maintaining open lines of communication with their medical team and understanding local laws and regulations around cannabis use.
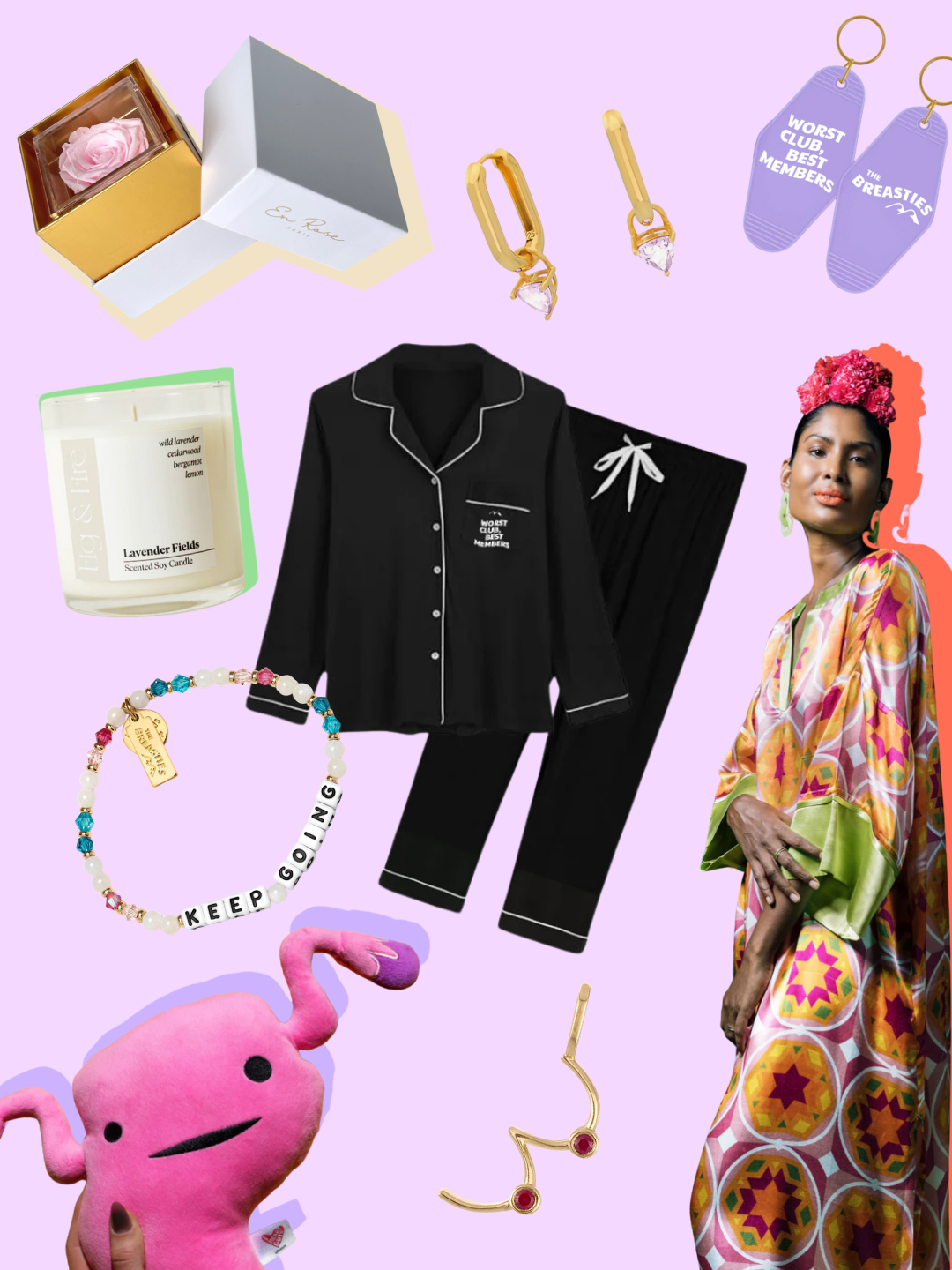
What do Breasties Have to Say About Cannabis?
Jaclyn, a 28-year-old previvor with the BRCA1 genetic mutation from Connecticut, used cannabis medicinally for years prior to their preventative mastectomy and salpingectomy, or the removal of the fallopian tubes, to manage symptoms related to other chronic illnesses. They were open with their medical team about their use of cannabis, which they say helped establish trust.
“Using cannabis helped me tremendously,” Jaclyn says. Incorporating cannabis products, like edibles and Rick Simpson Oil, reduced their reliance on opioids and gabapentin for managing post-operative pain.
“I got more restful sleep, had less blood pressure issues related to [postural orthostatic tachycardia syndrome], less constipation because opioids were no longer impacting my digestive system, and I actually had an appetite.”
“Cannabis helped me control my pain without the worry of other bodily processes being negatively impacted as a result,” they explain.
New Yorker Kristen, a triple-positive breast cancer survivor, found that working with her cancer center’s palliative care team to use cannabis for symptom management during chemotherapy helped her feel “very in control.”
Prior to chemotherapy, Kristen, 29, says that cannabis wasn’t for her, but a lack of appetite and feelings of anxiety opened her up to the idea. A palliative care doctor prescribed her a medical card and a dosage of one-to-one THC to CBD, to be taken through edibles or sublingual tablets.
“It helps me eat dinner. It distracts me enough,” she says. “It really does make me happier.”
Since adding cannabis to her post-chemo protocol, Kristen says she has regained the weight she lost when her appetite was reduced. “I can't imagine doing chemo without it.”
That said, Jaclyn reminds fellow Breasties to treat cannabis like any other prescription medication; use it responsibly, as you would other sedative or psychoactive medications, and keep it out of reach of children and pets.
“Be honest with your care team if you use it,” they say. “It can impact anesthesia for any procedure and it can’t be mixed safely with certain medications.”
When asked what she would say to fellow Breasties considering cannabis during cancer treatment, Jaclyn says, “Don't be afraid to ask for what you need.”
Despite cannabis still being taboo, Kristen says, “Just advocate for yourself. They're your doctor, they don't want you to suffer. Ask for what you need.”
What Questions Can You Ask Your Medical Team About Cannabis?
If you think cannabis might be helpful for you, Dr. Malhotra suggests asking the following questions to engage with your medical team and make an informed decision.
- What is the difference between cannabis vs a synthetic cannabinoid-containing medication?
- How beneficial is using cannabis or cannabinoids for my specific symptom/condition?
- What are the benefits and potential side effects of cannabis or cannabinoids, and how are they managed?
- Could I take cannabis or cannabinoids during active treatment without it interacting with any of my other medications?
- How will it affect my ability to do my daily activities, such as working and driving?
- Are there any long-term complications I should be aware of?
- Who would prescribe it and where would I get it?
- What are the local laws and regulations around using and carrying cannabis or cannabinoids?
- Where can I get more information?