Medically reviewed by Eleonora Teplinsky, M.D. and Dena Goldberg, MS, LCGC.
Gynecologic cancers is an umbrella term for cancer that occurs in the reproductive system of people assigned female at birth. There are five main types.
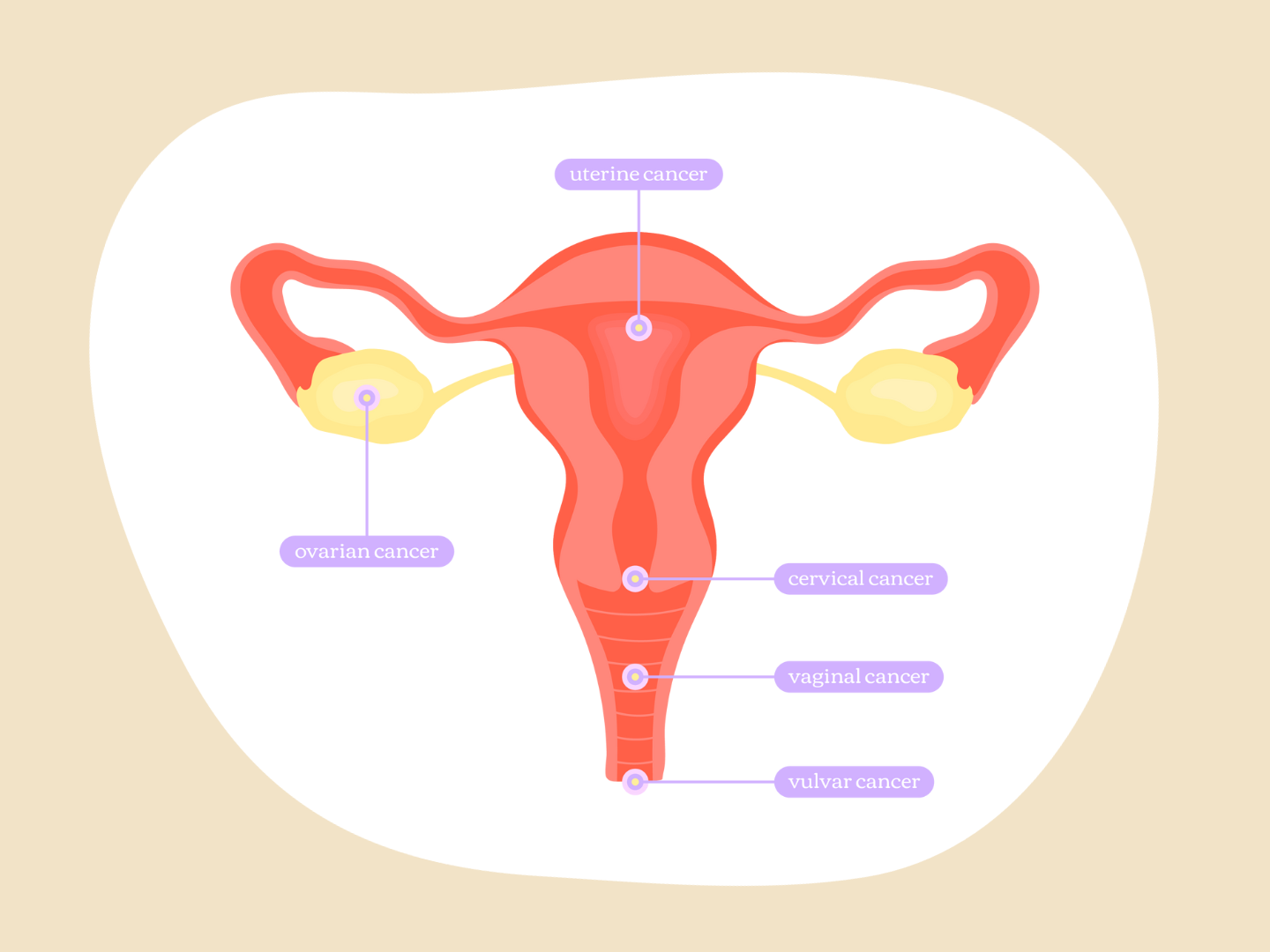
Ovarian Cancer
Cancer that develops in the ovaries, but also includes fallopian tube and primary peritoneal (tissue that lines the abdominal cavity) cancer, because they are treated in the same way. Types of ovarian cancer include:
- Epithelial,which accounts for the majority of ovarian cancers and includes high-grade serous, endometrioid, clear cell, mucinous, and low-grade serous carcinomas
- Germ cell
- Sex-cord stromal
Cervical Cancer
Cancer that develops in the cervix. Most cases are squamous cell carcinoma, but can also be adenocarcinoma, or cancer that develops in the glandular cells of the endocervix.
Uterine Cancer
There are two types of uterine cancer. Endometrial cancers, which develop from the lining of the uterus, are the most common, accounting for 95 percent of cases, while uterine sarcomas develop from the muscle in the wall of the uterus or nearby connective tissue. Types of endometrial cancer include:
- Endometrial carinoma
- Uterine carcinosarcoma
- Squamous cell carcinoma
- Small cell carcinoma
- Transitional carcinoma
- Serous carcinoma
- Clear cell carinoma
Vaginal
Cancer that develops in the vaginal canal.
Vulvar
Cancer that develops on the vulva.
Of the five, uterine cancer is the most common, followed by ovarian and cervical, while vaginal and vulvar cancers are quite rare, according to the U.S. Centers for Disease Control and Prevention (CDC).
What are the Risk Factors?
Hereditary Cancer Syndromes
There are genetic variations, also known as hereditary cancer syndromes, that can increase someone’s lifetime risk of developing ovarian and endometrial cancers, when compared to the average population.
The lifetime risk of epithelial ovarian cancer for the average population is between 1 and 2 percent, according to the National Comprehensive Cancer Network (NCCN). The following genetic variants can increase someone’s lifetime risk:
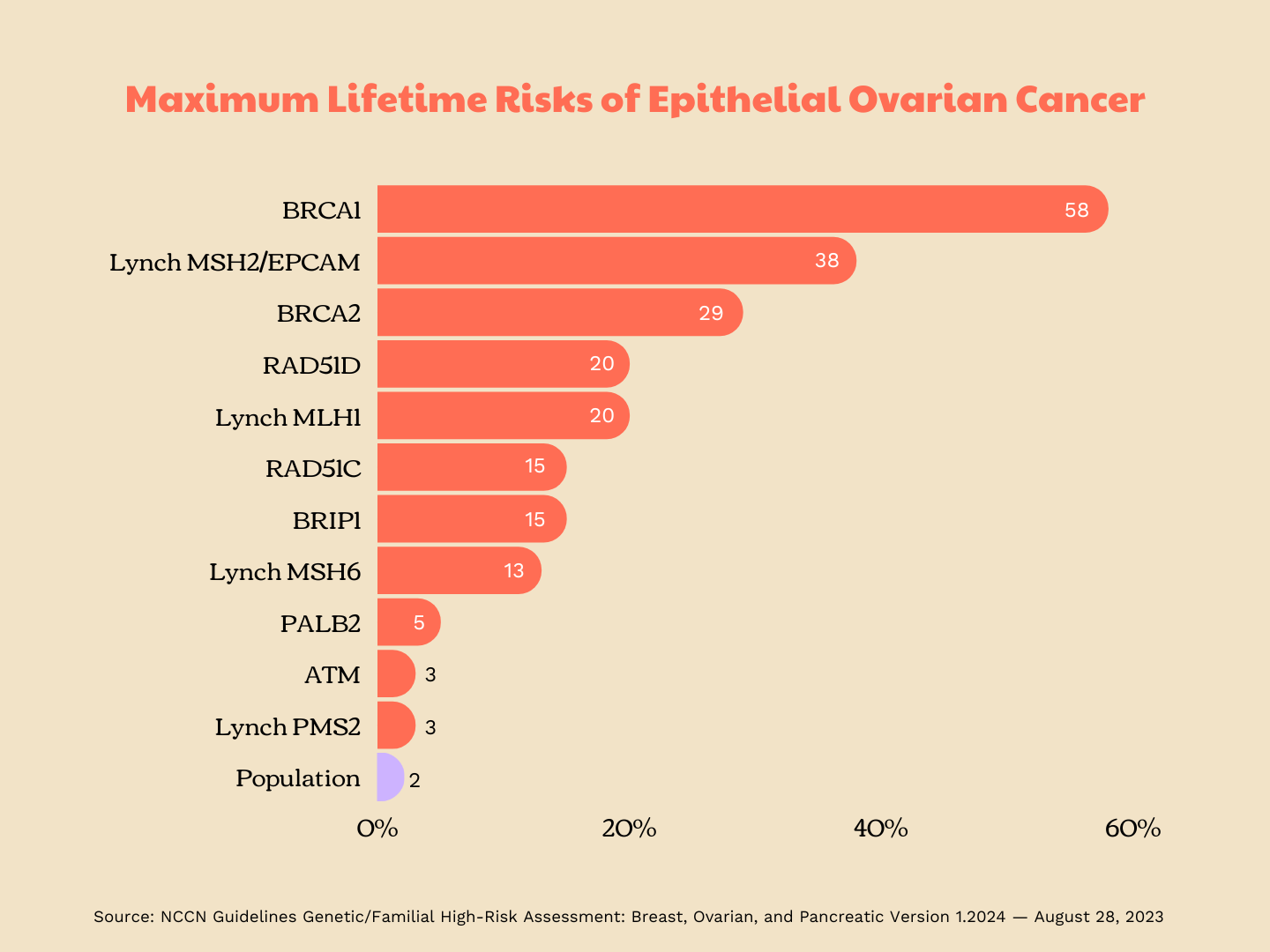
- ATM: 2-3%
- BRCA1: 39-58%
- BRCA2: 13-29%
- BRIP1: 5-15%
- Lynch syndrome (MLH1): 4-20%
- Lynch syndrome (MSH2/EPCAM): 8-38%
- Lynch syndrome (MSH6): ≤1-13%
- Lynch syndrome (PMS2): 1.3-3%
- PALB2: 3-5%
- RAD51C: 10-15%
- RAD51D: 10-20%
While the lifetime risk for endometrial cancer for the average population is 3.1 percent, says the NCCN, that increases to anywhere from 13 and 57 percent for those with Lynch syndrome and up to 28 percent for those with the PTEN genetic variant.
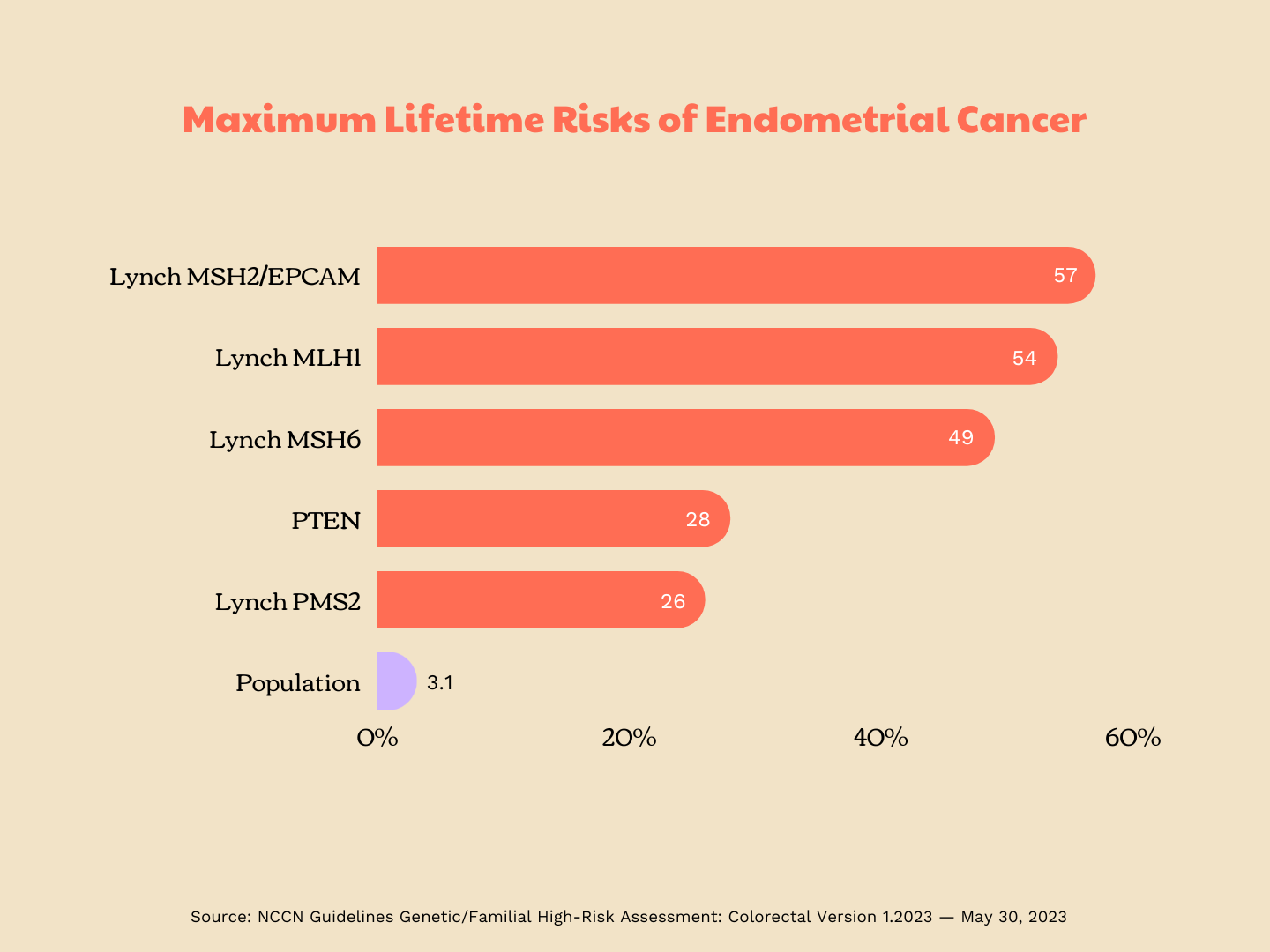
The specific lifetime risks for those with Lynch syndrome related genetic variants are:
- MLH1: 34-54%
- MSH2/EPCAM: 21-57%
- MSH6: 16-49%
- PMS2: 13-26%
Cervical, vulvar, and vaginal cancers, on the other hand, are rarely hereditary.
Other Risks
Other risk factors include human papillomavirus (HPV), a sexually transmitted disease. HPV is the main cause of cervical cancer, says the NCI, accounting for 70 percent of cases worldwide. HPV is also reported to cause 75 percent of vaginal and 70 percent of vulvar cancers.
Your physician may also look out for vaginal intraepithelial neoplasia (VAIN) and vulvar intraepithelial neoplasia (VIN) during routine gynecologic exams. These are abnormal cells that are not cancerous but may turn into cancer in some cases
What are the Symptoms?
It’s important to know your normal when it comes to gynecologic cancer because symptoms can often be vague and mistaken for something less serious. Some symptoms that may occur across multiple gynecologic cancers include:
- Abnormal vaginal bleeding, such as bleeding during intercourse or bleeding between periods
- Any bleeding after menopause
- Abnormal vaginal discharge, including changes in consistency or odor
- Pelvic or abdominal pain
- Pain during intercourse or urination
- New changes to bowel movements, such as constipation or diarrhea that does not resolve in 2 weeks
- New lumps in the vagina or on the vulva.
For vulvar cancers, symptoms can also include itching or burning sensation in the vulva, changes in color, or sores or ulcers on the vulva.
For ovarian cancers, other symptoms may also include persistent abdominal bloating, difficulty eating or feeling full quickly and/or feeling an urgent need to urinate or to urinate frequently.
New, persistent or worsening back pain may also be a symptom of advanced ovarian or cervical cancer.
How Can You Screen For and Prevent GYN Cancers?
Very few cancer types, such as breast, cervical, colorectal, and prostate, have a screening test recommended by the United States Preventative Task Force (USPSTF) for the general population (those who don't have a family history or genetic predisposition). This means that other types of cancer in the average individual are found by other means, emphasizing the importance of knowing what feels normal to you.
Cervical Cancer Screening
Regular Pap tests are recommended to screen for cervical cancer. While specific guidelines vary between organizations, it is generally recommended to have a first Pap test at age 21 and repeated every three years, with an additional HPV or HPV/Pap co-test after the ages of 25 to 30.
Because recommendations vary, it’s important to speak to your doctor to establish a screening plan that works for you.
Ovarian Cancer Screening
Screening for ovarian cancer is challenging.
Why? Current screening modalities-–a transvaginal ultrasound and a serum tumor marker cancer antigen 125 (ca-125) blood test—have a high-rate of false positives which can lead to unnecessary surgical interventions. That means that the harms can outweigh the benefits for average risk individuals.
Multiple studies have also found that although screening for ovarian cancer can detect early-stage disease, it does not reduce ovarian cancer mortality. As such, it is not recommended that those at average risk for ovarian cancer undergo additional screening.
It can be a little more complicated for those who are high-risk, who may feel that imperfect screening is better than no screening at all. It’s always a good idea to discuss the risks and benefits of screening with your healthcare provider to decide what’s best for you and where preventative surgeries may fit in.
Endometrial Cancer Screening
Though the symptoms of endometrial cancer can often be confused for something less serious, the NCCN reminds us that seeking care for symptoms that are abnormal for you allows for the cancer to be caught early.
They also say that patients with Lynch syndrome should consider an endometrial biopsy every one to two years starting between the ages of 30 to 35, or 5 to 10 years before the earliest age of diagnosis of Lynch-assoicate cancer of any kind in one’s family.
Preventing GYN Cancers
Because of the risks of cervical, vaginal, and vulvar cancer associated with HPV, one of the best protections against those cancer types is the HPV vaccine, Gardasil 9. While the CDC recommends vaccination around ages 11 or 12 and/or before a person is sexually active, it is approved for anyone below the age of 45.
Ovarian cancer can also be prevented through prophylactic surgery, a salpingo-oophorectomy or the removal of the fallopian tubes and ovaries.
For those with BRCA1 and BRCA2 pathogenic variants, a risk-reducing salpingo-oophorectomy is recommended between ages of 35 to 40 and 40 to 45, respectively – for those who are done with child bearing
Similarly, the NCCN also recommends a salpingo-oopherectomy and hysterectomy for those with Lynch syndrome who are done with childbearing.
Studies are also underway to understand whether the removal of the fallopian tubes on their own, a salpingectomy, is effective at reducing ovarian cancer risk while allowing patients to delay menopause. The motivation behind the research is that there are indications that the most common type of ovarian cancer starts in the fallopian tubes, rather than the ovaries themselves.
The American College of Obstetricians and Gynecologists (ACOG) recommends opportunistic salpingectomy to reduce ovarian cancer risk in patients who are having pelvic surgery and done with childbearing.
Other surgeries that could be used to prevent GYN cancers include:
- Supracervical hysterectomy: Removal of the uterus, with the cervix left in place
- Total or simple hysterectomy: Removal of the uterus and cervix
References
National Clinical Practice Guidelines in Oncology. Genetic/Familial High-Risk Assessment: Colorectal. Version 1.2023, 30 May 2023.
NCCN Clinical Practice Guidelines in Oncology. Genetic/Familial High-Risk Assessment: Breast, Ovarian, and Pancreatic. Version 1.2024, 28 August 2023.