The first step to advocating for the best care possible is knowing options, but figuring out where to start can be challenging.
To help break down barriers, leading researchers and healthcare providers made the trek to Camp Breastie in Rock Hill, NY, from June 1 to 4, 2023 to join those impacted by breast and gynecologic cancer for a four-day summit of connection and learning.
Through panel discussions and breakout sessions, subject matter experts shared the latest innovations and answered questions relating to everything from cancer screening and imaging, nerve preservation, genetic testing, fertility, and more.
Screening and Imaging
Catching Recurrence Earlier with Signatera
What if you could catch a recurrence before any symptoms appear?
According to Kevin Masukawa, VP of Marketing for Natera, a genetic testing company, this is possible thanks to circulating tumor DNA (ctDNA).
He explained that DNA can be found in the blood as a result of normal cells dying and shedding. He continued that the same process happens when cancer cells die, thus becoming ctDNA that can allow physicians to detect molecular residual disease with Natera’s Signatera.
Signatera is a blood test that is personalized, designed using a patient’s own tumor tissue.
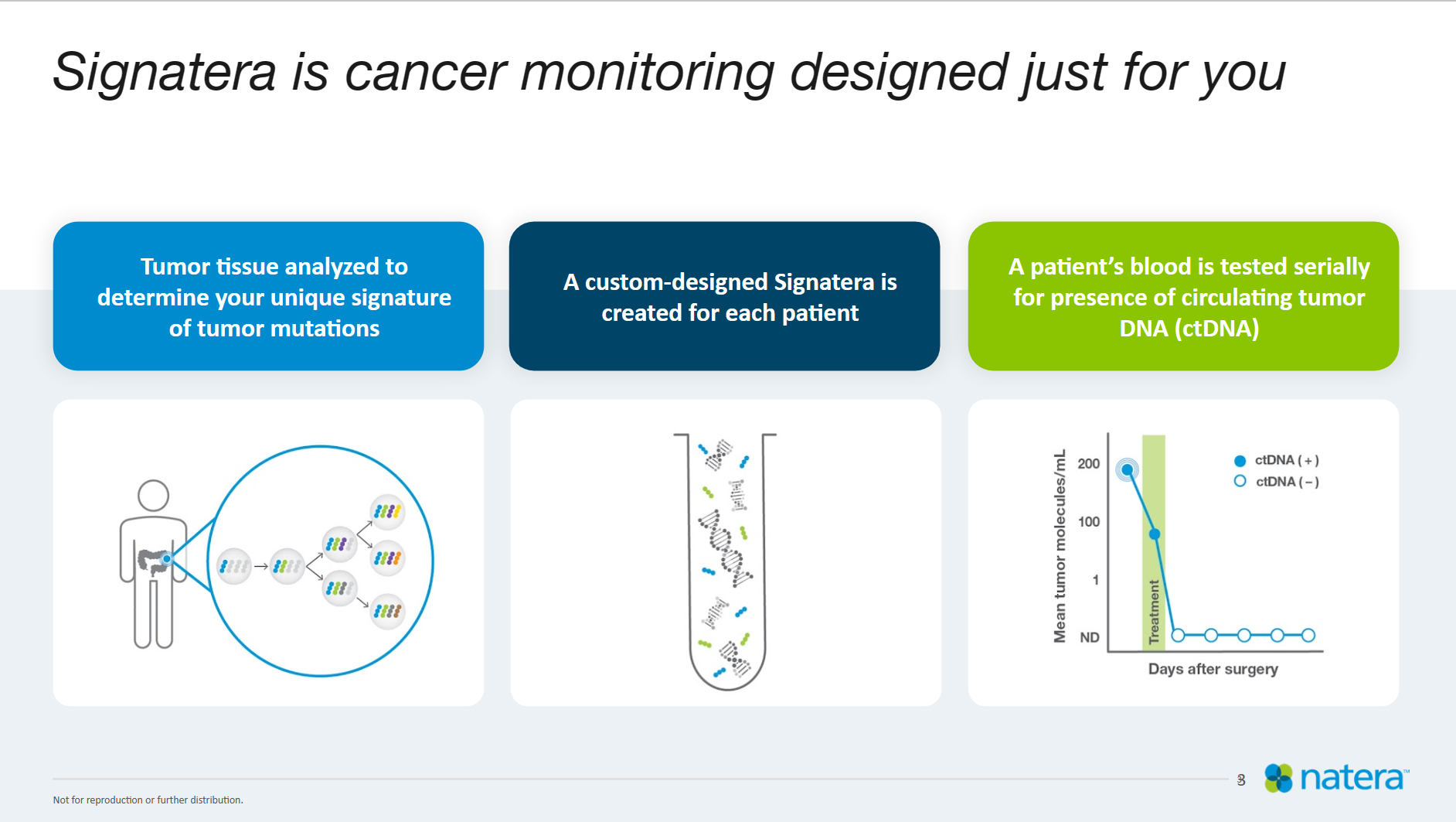
“We like to call it a fingerprint,” Masukawa said. “So just like each one of you in this room has a unique fingerprint, so does your tumor, and being able to identify that fingerprint for that tumor enables you to track that tumor over time.”
Doing so, Masukawa said, allows physicians to answer a slew of questions that may otherwise be difficult to explain with other technologies: “Is there cancer left in my body after surgery? Is my treatment working? And then finally, is my cancer coming back?”
Masukawa stressed the importance of working with one’s healthcare provider to understand what ctDNA testing–and a potential positive test–could mean for each individual.
“That's ultimately up to you and your clinician to decide whether or not this test might be right for you.”
Rethinking Approaches to Breast Imaging
“The problem with breast cancer imaging is that it's challenging,” said Dr. John Klock, a board-certified medical oncologist. “And the reason is cause the breast is all glands, so it’s very hard to see.”
To combat the challenges of imaging breast tissue, Dr. Klock, who has long been using his medical experience to innovate new technologies to improve health outcomes, has collaborated with the National Cancer Institute to develop new imaging techniques with 40 times the resolution of an MRI.
Watch the full Breastie Breakthroughs Panel Conversation
Called QT Imaging, the FDA-cleared device uses soundwaves as opposed to radiation, injection, or compression needed for scans such as MRIs, PET scans, or mammograms.
“Why do we need another breast imaging technology?” asked Dr. Klock. “Well, we need to detect really small cancers and we need a solution for dense breasts.”
The device, he explained, is more sensitive than other technologies, providing clinicians with 200,000 more data points when compared to an MRI. As a result, he explained, it “can generate a 3D model of the breast duct system in a living person,” which is integral to the treatment of breast cancer, which typically originates in the ducts.
In doing so, he said they are able to detect cancer more quickly and have fewer false results.
In efforts to make this type of imaging more accessible, Dr. Klock explained that because the device doesn’t need specialized training, like an ultrasound would, the scan can be installed in direct-to-consumer facilities outside of hospitals and cancer centers, which equally allows QT Imaging to bring the cost of a scan as low as possible.
Bringing Screening Out of the Hospital and Into the Home
Dr. Jill Dietz, a breast surgeon and past president and Chairman of the Board of the American Society of Breast Surgeons, said her approach to working with patients changed after witnessing her brother’s treatment for adrenal cancer.
“How I interacted with my patients was different because I understood,” she said.
But beyond that, she said, the experience pushed her out of the operating room, and though she said she misses her patients, “I want to make a bigger difference.”
Now as Chief Medical Officer and acting President of a Women’s Health start-up company, Cyduct Diagnostics, Dr. Dietz is focusing on developing an at-home test that examines biomarker profiles from fluid taken from the nipple called Be First.
Dr. Dietz explained that in a clinical setting, they are able to extract nipple fluid from 95 percent of people. From there, they can test for three biomarkers that are known to predict cancer.
“We want to empower you to take control over your own breast health and your breast risks, and then work with your healthcare team to be able to know what's going on in your breasts right now, a temporal assessment.”
This, she said, is one step in introducing biomolecular risk assessments as a clinical screening process.
“We want to put what we know works in a clinical setting and in a laboratory setting into the hands of individuals to help take care of and empower patients.”
Surgical Innovations
Preserve Feeling After a Mastectomy with Resensation
What happens when you cut the power cord of a TV? It might still be plugged into the wall, but there won’t be anything on the screen.
According to Emily Hansen, Senior Director of Resensation, that is similar to what happens when nerves are cut during mastectomies. The damaged nerve is still firing signals to the brain despite not picking up on sensations from the affected area, causing numbness or chronic pain, also known as post-mastectomy pain syndrome.

Enter Resensation and leading breast and plastic surgeons, such as San Francisco, CA-based Dr. Anne Peled and New York, NY-based Dr. Jonathan Bank. Together, they have been pioneering microsurgery techniques that use nerve grafts to preserve or restore sensation during or following a mastectomy.
“None of us picked this. None of us picked having cancer,” said Dr. Peled, who is also a breast cancer survivor and member of The Breastie’s Board of Directors. “We all deserve the life we want.”
The key to sensation-preserving mastectomies is two-fold, Dr. Peled and Dr. Bank explained. The first step is planning an oncologically-safe surgery that saves or minimally damages as many nerves as possible, particularly those under the skin. The second step is using nerve grafts to lengthen and add flexibility to the nerves that were cut so that they may be reconnected.
How can a patient push for a sensation-preserving mastectomy? Talk to your team, said Hansen, Dr. Peled, and Dr. Bank.
“It’s a huge part of your quality of life,” urged Hansen.
“We can do all the teaching in the world to surgeons, but patient advocacy is what matters,” Dr. Peled said.
People impacted by breast cancer in the United States can also use Resensation’s Find a Surgeon tool to locate a qualified surgeon in their areas.
New Techniques Pushing for Lymphedema Prevention
Lymphedema is a chronic swelling that occurs when lymphatic vessels are not able to properly drain fluid in certain areas of the body. While not a given, lymphedema could become a concern for those who have undergone lymph node dissections or biopsies as a part of their cancer treatment.
Historically, lymphedema prevention has been limited to restricting heavy lifting, avoiding injuries such as needles and sunburns, and wearing compressive garments during high-intensity movement.
But using microsurgical techniques, similar to those used for nerve preservation, Dr. Peled explained, we “can channel around the areas, figure out which lymphatic vessels we can preserve, still take the lymph nodes we need, but instead channel these lymphatic tissues to go through vessels and go through veins.”
But moving upstream, Dr. Peled said, is considering whether an axillary surgery can be avoided in the first place. She explained that approximately 80 to 85 percent of patients who undergo lymph node surgery are doing so unnecessarily.
To avoid this, she said, surgeons can inject a tracer called MagTrace at the time of the breast surgery. The tracer will stay in the lymph nodes for 30 days, allowing surgeons to receive final pathology to determine if a lymph node biopsy is needed at a later date.
“This is so incredibly game-changing,” said Dr. Peled.
Diving Into Your DNA
“Genetics is the future of personalized medicine,” said Dena Goldberg, a certified genetic counselor and content creator whose mission is to educate the public and physicians about the importance of genetic testing.
When it comes to cancer, Goldberg explained, about 10 to 15 percent are hereditary, though rates vary by cancer type.

How does this happen? Goldberg explained that typically when a genetic mutation occurs, there is a backup of that gene that makes the mutated gene redundant or allows for the body to correct itself. When there isn’t a backup, however, the mutation can become cancer.
And why does knowing your genetic status matter? Genetic testing allows for risk management, Goldberg explained.
For example, she said, those who are at high risk of breast cancer can begin screenings with annual MRIs at 25 years old and mammograms at 30, rather than waiting until 50 years old as is recommended for those with an average risk.
Beyond that, Goldberg shared that genetic testing can also allow for a targeted treatment plan in the event of a cancer diagnosis, such as the use of PARP inhibitors in the treatment of BRCA-related ovarian cancers due to their ability to preferentially attack cancer cells with a BRCA mutation.
And when it comes to accessing testing, Goldberg explained that National Comprehensive Cancer Network (NCCN) guidelines say that anyone under 50 with a breast cancer diagnosis should be offered genetic testing. She also explained that “cost should never be a barrier,” as testing shouldn’t cost more than $250 regardless of insurance coverage.
Goldberg also urged that people should be tested for a full panel, beyond BRCA variations, citing Lynch syndrome as another common genetic variant with cancer links that impact approximately 1 in 280 people.
“Everybody deserves to get tested if they want.”
Research Moving the Needle on Breast Cancer Treatment
“Research brings a change,” said Dr. Steffi Oesterreich, Director of Education Women's Cancer Research Center, Magee-Womens Research Institute, and the recipient of the Breastie’s annual $50,000 stage 4 breast cancer research grant.
While much of the work Dr. Oesterreich looks at is still in the early stages, she shared that there is promising research that is improving outcomes for those with metastatic disease.
In the case of HER-2-positive metastatic breast cancer, one such area of focus is related therapies called antibody drug chemotherapy (ADC).
She explained that in conjugating, or attaching, the chemotherapy to an antibody, the drug becomes very effective, so much so that, “This is the first time ever that in the metastatic setting we talk about curing patients.”
“This hasn't happened before,” said Dr. Oesterreich. “I think these new ADCs therapies are an absolute breakthrough. I think this has changed the outcomes.”
Another important area of focus, Dr. Oesterreich shared, is lobular breast cancer. Although it has not yet been recognized as a disease distinct from ductal breast cancers, she explained that “clinically, they are very different.”
A hallmark of lobular breast cancer, she explained, is a molecule that acts like a glue causing cells to stick together making them harder to pick up on imaging. Once metastatic, Dr. Oesterreich said, the disease continues to behave differently, spreading to atypical sites in the body. As such, to improve outcomes for lobular breast cancer, more research is needed.
Further, she said, they want patient advocates to share wants important to them, inviting folks to join researchers at the International Invasive Lobular Breast Cancer Symposium (ILC) in Pittsburgh, PA in September 2023.
However, Dr. Oesterreich stressed, progress can only be made if researchers have access to disease tissue. Though an uncomfortable topic, she explained that researchers are incredibly grateful for those who donate their bodies at the time of death to hopefully enable advancement for those who come after them.
“It’s one of those projects where we as researchers feel a tremendous responsibility to make the absolute best use of those tissues for state-of-the-art approaches.”