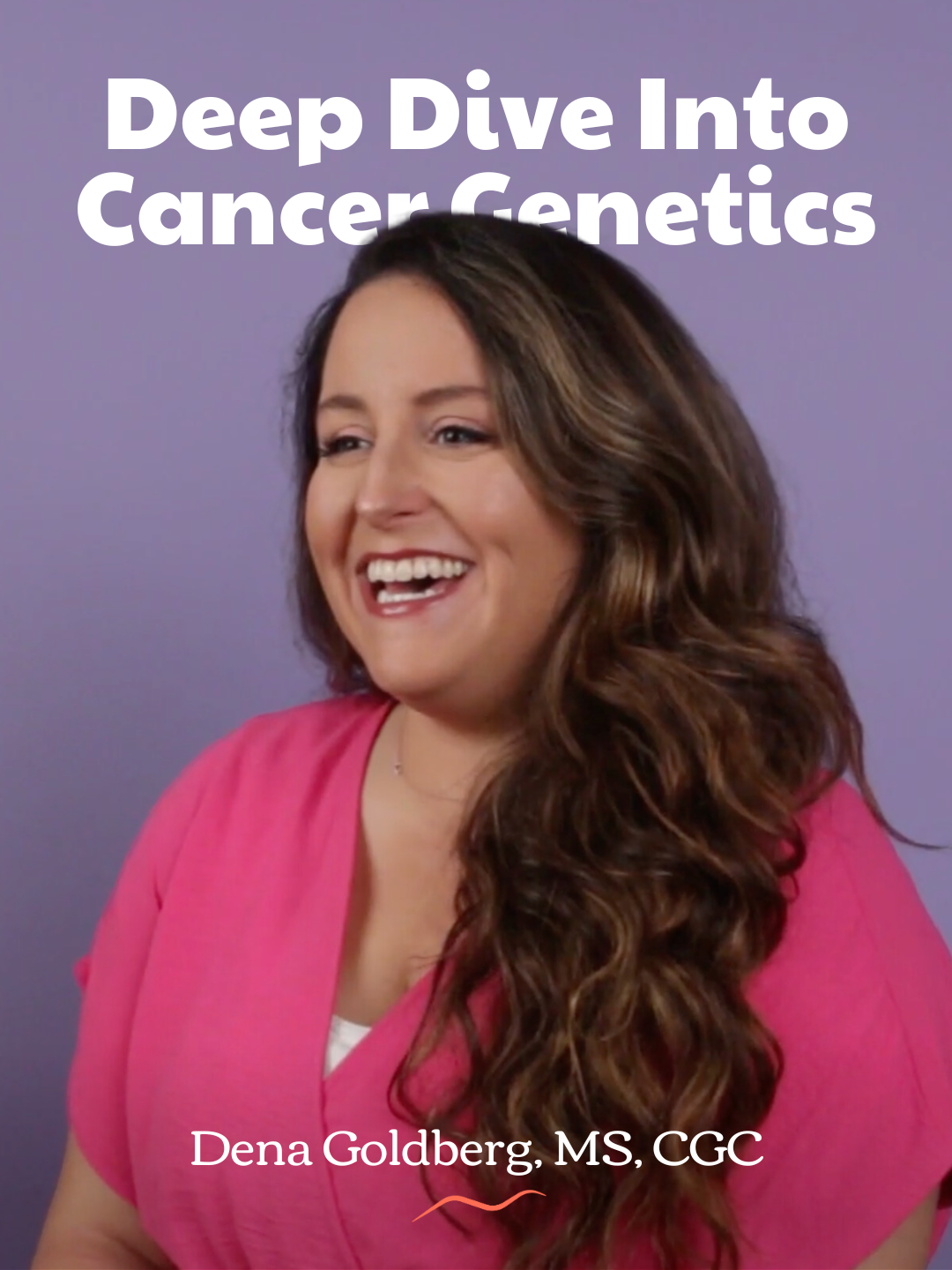
Olivia Munn’s announcement that she was diagnosed with breast cancer earlier this year struck a particularly painful chord for me. Like her, I recently underwent genetic testing due to my extensive family history of the disease. Like her, my results were clear. I was what geneticists call a ’true negative’ for all known breast cancer gene variants, including CHEK2, which a number of women in my maternal line carry.
There was, however, a catch.
The CHEK2 variant comes with a 20 to 40 percent lifetime risk of developing breast cancer, lower than the 60-70 percent associated with the BRCA1 and 2 variants, but every woman in my family who carries the variant has been diagnosed with the disease, some of them in their 30s. I ultimately received the same news as Munn: With a family history like mine, a negative genetic test didn’t automatically make me low risk. I needed a full risk assessment.
Use a Breast Cancer Risk Assessment to Paint a Full Picture
Munn has not shared the specifics of her family history, but she has identified it as a factor that led to her classification as high risk.
The Tyrer-Cuzick model, the risk calculator used by both my and Munn’s doctors, utilizes multiple risk factors to assess someone’s lifetime chances of developing breast cancer. Non-familiar factors include breast density, lifestyle and dietary habits, and personal history of noncancerous breast diseases. On the familial side, the model requires a detailed history of all family cancers, logging the age of each relative at diagnosis, their gene status, and the outcome of their illness. The CDC defines high risk status as anybody with a calculated lifetime risk of higher than 20 percent. My own score was 31 percent, a little lower than Munn’s 37. Neither of us carried a genetic variant, but both of us were high risk anyway.
Neither of us, as it turns out, is an anomaly.
Danielle Dondanville, a genetic counselor at Cedars-Sinai Medical Center in Los Angeles, CA, explains that while around around 5 to 10 percent of individuals diagnosed with breast cancer are found to carry a gene variant that increased their risk of developing the disease, “in the vast majority of breast cancer cases, we do not identify a single gene variant or problem as the explanation for one’s diagnosis.”
“In these cases, we know that there are a variety of risk factors that contribute to one’s risk for developing breast cancer,” she says.
Alongside the factors used by the Tyrer-Cuzick model, Dondanville says “it’s certainly possible that in some families with suspicious family history of breast cancer … that there are variants that current technology is unable to detect, or genes to explain the history that we’ve yet to discover.”
Haylee Kline is also gene negative, but recently learned she has a 48 percent lifetime risk of developing breast cancer. She says she “had no idea that there were so many other genes that played a role.”
“I knew that my family history would make me high risk but I had no idea that my risk could double without having the gene,” said Kline, who is currently recovering from a risk-reducing mastectomy, lowering her risk level to less than 5 percent.
Look Beyond BRCA Variants
Dondanville finds that patients are most likely to be familiar with BRCA 1 and 2, as opposed to other variants. This isn’t surprising: they’re the most common genes linked to breast cancer, they’ve benefitted from wide media coverage, and clinical testing for them has been available since the 1990s.
The problem is the prevalent belief that if someone tests negative for BRCA 1 and 2, they don’t need to worry about hereditary breast cancer.
Erin Bergen, who carries the ATM variant, says “nobody ever suggested” she needed genetic counseling, despite a family history riddled with cancers. It was not until her first mammogram that a doctor suggested she meet with a genetic counselor.
Bergen and her sister both tested positive for the ATM variant. At her sister’s subsequent MRI screening, she was diagnosed with breast cancer.
“[We] definitely have to advocate for ourselves,” says Bergen, who has now undergone a prophylactic mastectomy and hysterectomy.
Advocate for Yourself, No Matter Your Age
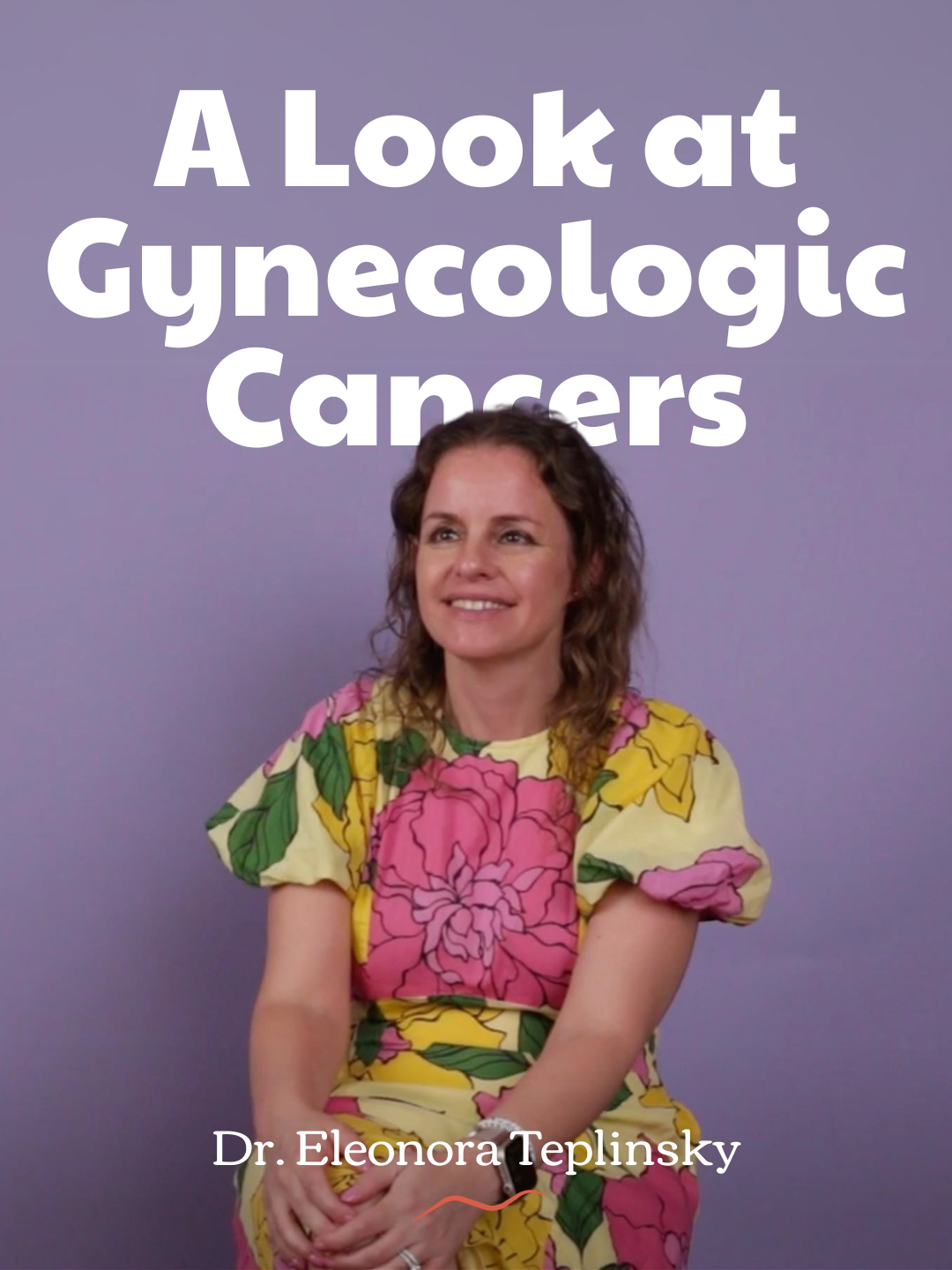
In response to the rise in breast cancer diagnoses in young patients, the US Preventive Services Task Force recently recommended that women with no identified risk factors for breast cancer get their first screening mammogram at 40, a decade earlier than the previous recommendation of 50.
In terms of early diagnosis, it’s a step in the right direction, but genes and genetic predispositions don’t wait, and younger patients are particularly vulnerable to inherited cancers. If a woman under 40 is assessed as high risk, she can opt into high risk surveillance, which usually entails alternating mammograms and MRIs every six months, or undergo preventative surgery.
Without that knowledge, and the subsequent access to early screenings, patients are on their own. Research suggests around 80 percent of young patients find their breast abnormality themselves.
Amanda Nizewitz found a lump behind her nipple when she was 34. She was diagnosed with a benign adenoma and successfully underwent surgery and nipple reconstruction. Subsequent mammograms led Nizewitz’s doctors to discover multiple precancerous conditions, including lobular carcinoma in situ (LCIS), and her risk level was assessed at 50 percent. She was offered Tamoxifen, a drug that blocks estrogen and is used in the treatment and prevention of breast cancer, but ultimately decided to proceed with preventative surgery.
I was also offered Tamoxifen and high risk surveillance, but chose to undergo a prophylactic mastectomy.
That’s where my story differs from Munn’s. I was lucky—luckier than her, and luckier than all the women in my family who had no choice but to fight. My post-surgery pathology report revealed a few tiny cellular changes in my left breast. It’s possible that I was a ticking time bomb all along.
Munn has urged women with concerns about their family history to speak with their doctors about genetic counseling and risk assessment.
Dondanville has a similar message, and emphasizes that research into breast cancer-related genes is ongoing; anybody with a clear genetic test should check in regularly with their provider to find out what new testing is available.