Peak Partnered: This article is in proud partnership with Resensation. Resensation and The Breasties are teaming up to increase education around post-mastectomy sensation loss for anyone impacted by breast cancer.
The History of Mastectomy Surgeries
In 1804, the world’s first surgery under anesthesia was performed. It was a mastectomy performed by Japanese surgeon, Seishu Hanaoka.
But where are mastectomy surgeries now? Thankfully, they have come pretty far but some would argue that they still have a ways to go.
In fact, studies show that as breast oncologic surgery evolved throughout the 19th century, a long period of confusion over techniques and effectiveness persisted.
In 1882, William Halsted established the radical mastectomy in the United States which was an aggressive procedure involving the complete removal of the breast, skin, chest muscles, and lymph nodes. In 1972, John Madden modified the radical mastectomy to be more conservative by highlighting the preservation of both pectoral muscles.
In recent years, there has been a push to understand the impact and side effects of mastectomy surgeries. One important area that advocates are hoping more care teams address is the loss of sensation and chronic numbness following a mastectomy surgery. Nerves cut during a mastectomy can mean living the rest of your life with a numb or partially numb chest.
Understanding Why Post-Mastectomy Sensation Loss Happens
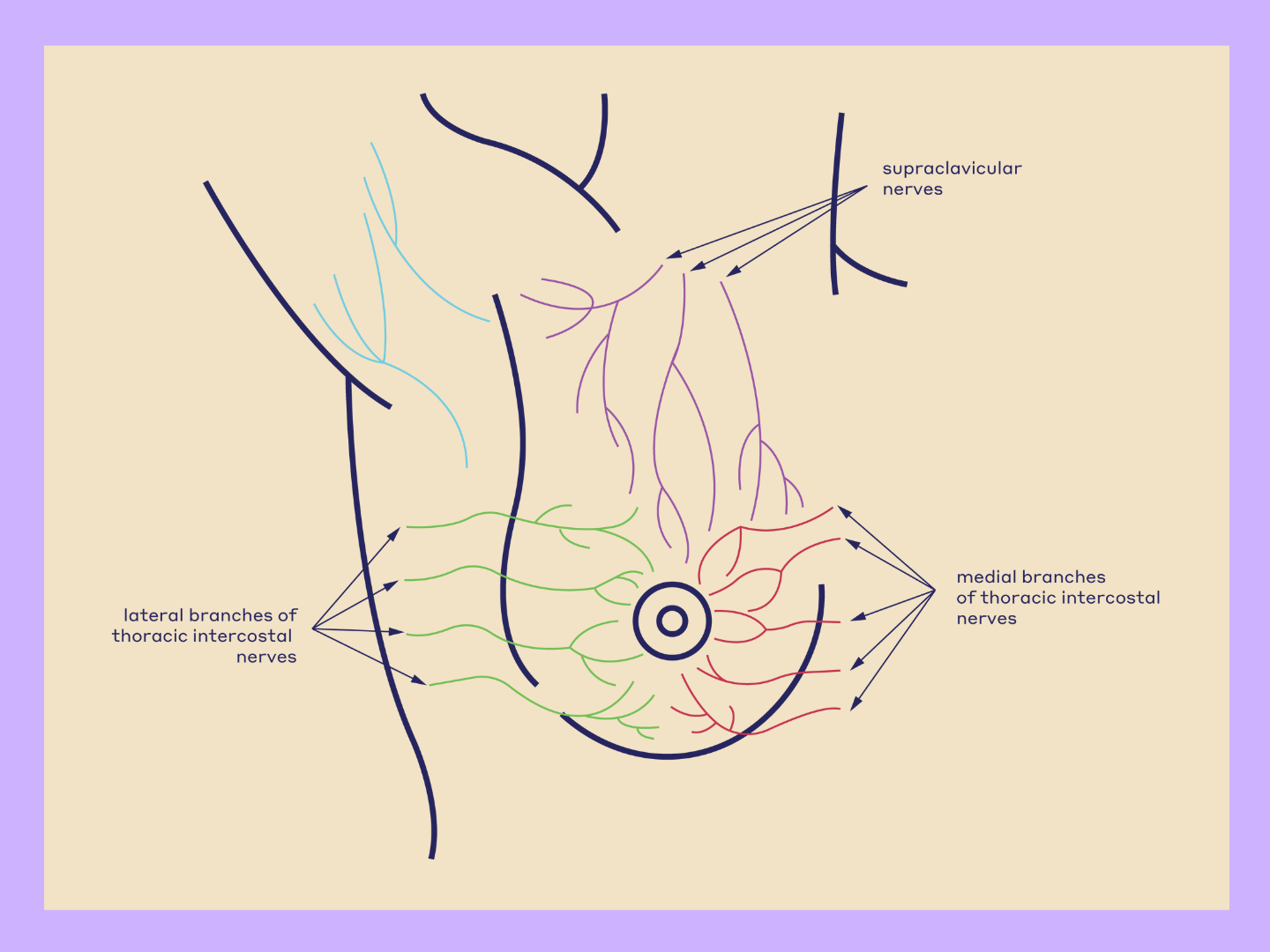
Peripheral nerves run through every part of the body and allow interaction with the outside world. They act like wires, carrying signals to and from the brain throughout the entire body. Motor nerves carry messages from the brain to muscles to make the body move and sensory nerves send signals back to the brain, carrying the messages that allow you to feel.
“There are sensory nerves in the breast that allow you to feel touch, temperature — and even pain. During a mastectomy, the sensory nerves are cut when the rest of the breast tissue is removed," says Dr. Michael Mirzabeigi, plastic and reconstructive surgeon from Atlanta Plastic Surgery.
"It’s a bit like cutting the power cord to your TV, it interrupts the electrical signal. Nerves in the breast are similar. Once cut during a mastectomy, the signals cannot communicate back and forth, which can leave a patient’s chest partially or completely numb. This is the case for both standard mastectomies, as well as nipple-sparring mastectomies," he explains.
According to new research, patients often say they weren’t prepared for how numb they would feel after mastectomy or just how much it would impact their daily lives. (1)
Unsurprisingly, the loss of breast sensation and the subsequent numbness that many people experience can be disruptive to body image, intimacy, and quality of life. (2) Research published in 2016 in The Journal of Breast Health examined quality of life in breast cancer patients and found that all 20 participants reported negative experiences and emotions following their mastectomy surgeries resulting from physical changes of the operation.
Some of the Challenges of Living with Chest Numbness
“Touch is such an important part of our everyday lives that many of us take for granted. Hugging a loved one, getting dressed, and really just feeling normal are a huge part of how we interact with the world around us," says Dr. Mirzabeigi.
"It’s hard to explain to someone what losing the ability to feel a part of your body might be like, it can be hard to comprehend what sensation loss may mean long-term, but for many women it really impacts their quality of life and their ability to feel normal after cancer."
Without the ability to detect touch, there can be feelings of disconnectedness to your chest. Additionally, without sensation, you may not feel changes in temperature.
A June 2021 study published in the Aesthetic Surgery Journal examined 28 cases of burn injuries in breast reconstruction patients. Study authors concluded that loss of sensation is not only irksome for patients, but can also disguise burns occurring in the breast and advised all patients undergoing breast reconstruction to be aware of the increased risk and stay away from dark-colored bathing suits. One can imply that this might be an important warning due to the lack of feeling following a mastectomy and the inability to feel temperature changes.
A 2016 article published in the journal of Plastic and Reconstructive Surgery highlights that sensation is decreased or completely gone following breast reconstruction and leaves breasts vulnerable to injury from common household thermal sources like heating pads and hot water bottles, as well as the sun. This study also advises medical professionals to advise patients of the increased burn risk.
Personal Experiences of Navigating Chest Numbness
What other challenges do patients face when navigating chest numbness after a mastectomy? Here’s what a few community members had to say:
Rachel Furtney, 29, preventative mastectomy patient
“One of the biggest challenges following loss of sensation is dealing with carrying things between my arms and chest. I carried a bottle of wine between my arm and chest and did not feel it start to fall until it was too late,” says Rachel Furtney, 29, who had a preventative mastectomy at age 26.
Kelsey Litwin, 27, breast cancer patient
“Losing sensation post-mastectomy is a very jarring experience. It’s really strange to be able to touch but not fully feel a part of your body — especially one that was at one point linked both to pleasure and trauma. Even though I now know what to expect, almost two years later, the numbness still catches me off guard,” says breast cancer survivor Kelsey Litwin, 27, who had a mastectomy at age 25.
Kellie Goss, 51, preventative mastectomy patient
“One of the most challenging things to get used to after my prophylactic surgery is the loss of sensation in my breasts. My surgery was nipple-sparing, so my breasts look the same as they’ve looked all of my life and the expectation was that they’d feel the same also. Not. The. Case. It certainly took a lot to get used to as I battled the phantom itch that I just couldn’t scratch and learned to settle into my new normal. Admittedly, I still long for the closeness that comes from a hug from a friend and I wish I had that pillow-like effect when my daughter comes in for an embrace. I miss those things most of all, but I am comforted by the knowledge that I’m still here to celebrate the things that matter most.” Kellie Goss, 51, who had a preventative mastectomy at age 47.
Bianca Muńiz, 27, three-time cancer patient
“Bumping into things has been challenging. I bumped into Donnie (my boyfriend) and he spilled something on me and I had no clue. Also when I'm wearing low neck clothing, I'm so stressed about my boob flashing that I'm constantly readjusting and looking down and just stressed,” explains Bianca Muńiz, 27, who was diagnosed with breast cancer and had a mastectomy at age 22.
Mary Dee, 45, breast cancer patient
"My doctor did great work but there wasn't any real conversation around whether I would or wouldn't have sensation. In my right breast I still have no sensation and in the other side I get what can only be described as a chill anytime something touches my left breast. The nerves want to work, but someone has to know how to make that happen. I have hope for the future that this can be restored,” says Mary Dee, 45, who was diagnosed with breast cancer at age 40.
Restoring Sensation During Breast Reconstruction
Living with a numb chest doesn’t have to be the norm. Restoring sensation during breast reconstruction is possible through a surgical technique called Resensation.
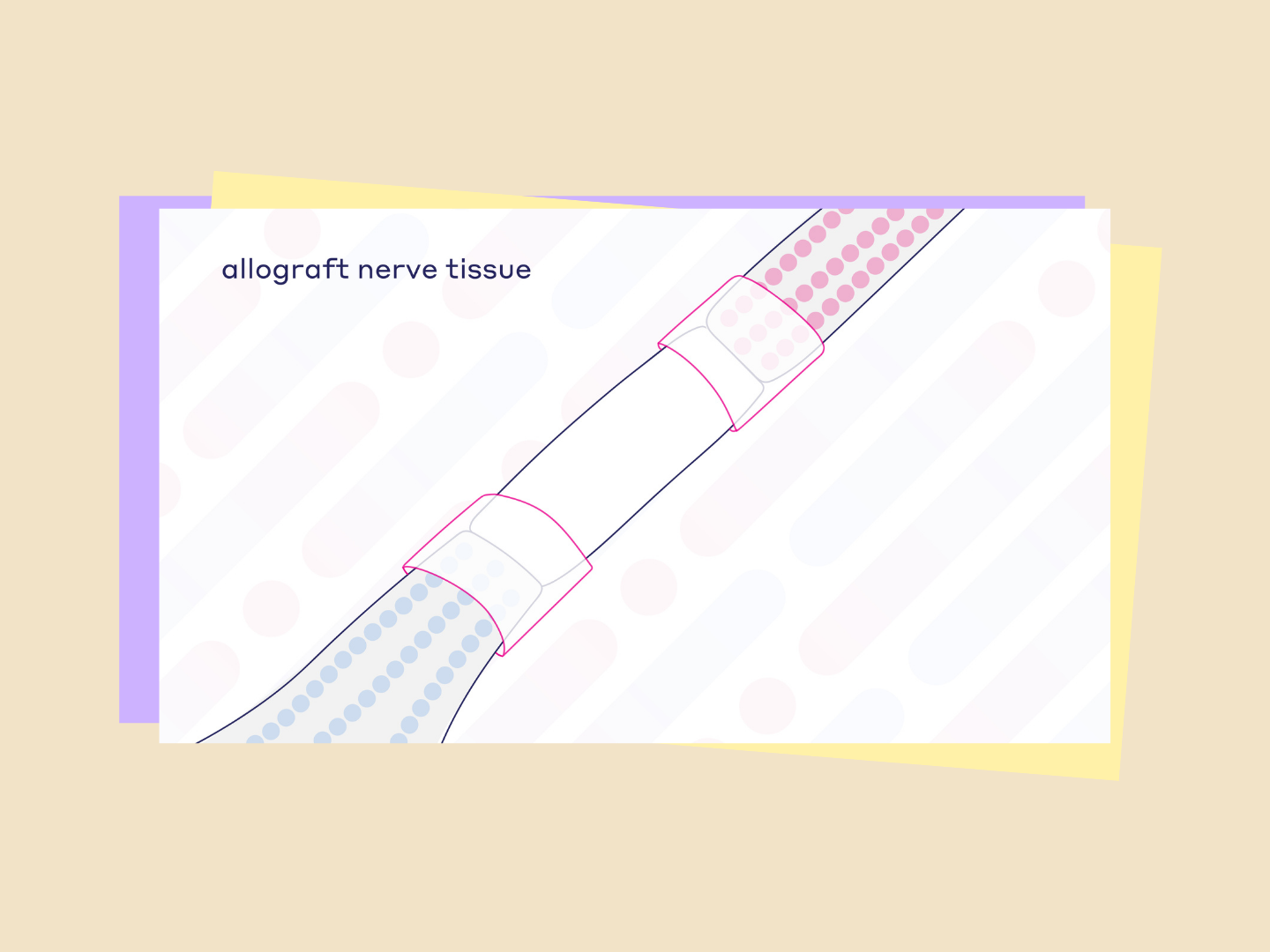
“During Resensation, nerves cut during the mastectomy are reconnected using allograft nerve tissue. Over time, the nerve regenerates, potentially restoring sensation and becoming a part of the patient’s body in the process. " says Dr. Joshua Lemmon, plastic and reconstructive surgeon of the Regional Plastic Surgery Center in Dallas, Texas.
"Resensation can be done during an immediate or delayed reconstruction and may also be possible as part of a revision surgery to previous implant reconstruction," he explains.
In a recent study, women report that regaining sensation helps them recover and move on from their experience with cancer, the mastectomy and reconstruction process. It also helps them feel more normal and more like their old selves. (1)
As part of the study, 97 percent of patients interviewed who underwent Resensation:
- Would recommend that a friend or family member explore neurotization options.
- Said potential rewards in terms of physical and emotional impact and quality of life outweighed potential risk of the procedure not being successful.
- Believe that restoring breast sensation should become standard of care for breast reconstruction.
A study published in July 2019 in the journal Plastic and Reconstructive Surgery demonstrates that combining oncologic, reconstructive, and peripheral nerve surgery leads to improved sensory outcomes. The 16 patients included in this study who underwent a nipple-sparing mastectomy with direct-to-implant reconstruction experienced a 90 percent rate of preserved sensation.
How to Find the Right Medical Team
“Nerves are tiny intricate structures that must be handled with delicacy and precision. Performing Resensation requires a surgeon to be experienced with microsurgery" explains Dr. Lemmon. "Surgeons like myself, who are able to perform this procedure, have undergone specialized training to be able to repair blood vessels, nerves, and other intricate structures using a microscope and microsurgical instruments."
To find a surgeon who performs Resensation near you, visit the Resensation surgeon locator and browse providers by state.
The Importance of Self-Advocacy
More medical care teams need to know that numbness is a problem to help make the opportunity to regain sensation a standard of care for everyone undergoing breast cancer surgery.
A few tips to remember when advocating for yourself in a healthcare setting:
● This is your journey. As you discuss your options with a qualified care team, never be afraid to speak up, push for more answers and express what really matters to you.
● The more patients who ask about possibilities for restoring sensation, the more surgeons will realize that sensation loss is a widespread issue.
● Never underestimate the power of asking questions.
● Asking about it helps improve the level of advancement for everyone.
To learn more about sensation loss check out this video and head to www.resensation.com to read patient stories and learn more.
Sources and Fact-Checking
- Crohan S, Campbell A. Breast Sensations Research Report. Inspired Health. October 2020. Report on file at Axogen.
- Koçan S, Gürsoy A. Body Image of Women with Breast Cancer After Mastectomy: A Qualitative Reseach. The Journal of Breast Health. October 2016.
- Freeman MD, Gopman JM, Salzberg CA. The evolution of mastectomy surgical technique: from mutilation to medicine. Gland Surgery. June 2018.
- Bijkerk Ennie, Beaugels Jop, et al. Breast Sensibility After Mastectomy and Implant-Based Breast Reconstruction. Breast Cancer Research and Treatment. June 2019.
- Habibi K, Delay E, Sarfati I, Duteille F, Clough KB, Atlan M. Lessons Learned From Twenty-Eight Cases of Burns Following Breast Reconstruction: An Underestimated Complication Requiring Inclusion in Consent Information. Aesthetic Surgery Journal. June 2021.
- Faulkner HR, Colwell AS, Liao EC, Winograd JM, Austen WG Jr. Thermal Injury to Reconstructed Breasts from Commonly Used Warming Devices: A Risk for Reconstructive Failure. Plastic and Reconstructive Surgery. October 2016
- Peled AW, Peled ZM. Nerve Preservation and Allografting for Sensory Innervation Following Immediate Implant Breast Reconstruction. Plastic and Reconstructive Surgery. July 2019.